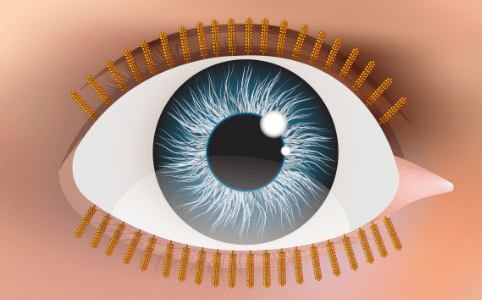
Did you know that your eyelids contain tiny oil glands?
These oil glands are known as Meibomian Glands. They are like pores in your skin.
Just like pores help to prevent your skin from drying out, Meibomian Glands help to keep your eyes moisture in balance.
How do oils help your eyes?
Each time you blink, your eyelids squeeze out fresh oil to evenly coat your eyes.
Although it’s an extremely thin layer, around 100nm, this layer is important.
This oil layer helps to:
- Protect your eyes from bacteria and debris
- Keep your eyes from feeling smeary or filmy
- Maintain comfort during a blink
What is Meibomian Gland Dysfunction?
Meibomian Glands may be tiny but they have a big job.
When they’re rendered inactive, your tears evaporate too quickly, leading to uncomfortable, sore or blurry eyes.
Meibomian Gland Dysfunction (MGD) is one of the most common causes of Dry Eyes. Up to 86% of patients diagnosed with dry eyes have MGD.
In short, MGD describes blockage or reduced quality of oil that affects your eyes.
Left untreated, MGD can lead to clogging and shrinking of your oil glands over time. So how can you prevent permanent change to your Meibomian Glands?
Today, we’re taking a deep dive into MGD. We’ll discuss causes, symptoms, and which treatment options are available to help.
Ready to learn more? Let’s dive in!
The Function of Your Meibomian Glands
Before we delve into the specifics of MGD, let’s review what your meibomian glands do and why they’re so important.
You’ll find these oil-secreting glands along your upper and lower eyelid. Your upper eyelid has about 25 to 40 individual glands, while your lower eyelid has 20 to 30.
They owe their complex name to Heinrich Meibom, a German doctor who first noticed and drew images of them back in 1966.
In addition to causing dry eye, MGD can also cause your eyelids to become inflamed, leading to a condition known as blepharitis.
Risk Factors for Meibomian Gland Dysfunction
As with all healthcare, knowledge is the key to prevention. If you know ahead of time that you’re at risk of developing MGD, you can take earlier steps to help combat and reverse the condition.
To this end, let’s review a few known risk factors that can contribute to MGD.
- Age
The older you get, the more you’re prone to dry eyes. This is because the senior population is more likely to experience one or more of the following conditions, which can upset a healthy ocular surface:
- Polypharmacy (taking multiple drugs to treat one condition)
- Androgen deficiency
- Lower blink rates
- Oxidative stress
As such, people over the age of 40 are more susceptible to MGD than younger populations. In fact, in one study of 233 older adults, researchers found that 59% showed at least one sign of MGD.
- Ethnicity
Data suggests that one’s ethnic background also plays a role in determining the risk factor for MGD. Specifically, Asian populations appear to be especially vulnerable. One study found that 46% to 69% of patients in Japan, Thailand, and China suffer from the condition. This is in comparison to 3.5% to 20% of Caucasians who have the condition.
- Eye Makeup
Do you wear heavy eye makeup on a regular basis? If so, the cosmetics can clog the opening of the meibomian glands and affect their performance. Chemicals in cosmetics can also be toxic to your eyes. Check out this post for some of the main ingredients to avoid. This is one more important reason why you should always remove all of your makeup before going to bed! Non toxic removers like Micellar Water or WeLoveEyes work great.
- Contact Lenses
More conclusive research is required before an official relationship can be drawn, but researchers believe there may be a correlation between contact lenses and MGD.This is because the lenses themselves can disrupt the glands, changing their functionality.
Relationship with Other Medical Concerns
When you suffer from MGD, you’re also more vulnerable to other medical concerns, not all of which are eye-related. Here are a few to keep in mind.
- Allergic conjunctivitis and other eye diseases
- Ocular Rosacea
- Autoimmune diseases (including rosacea, rheumatoid arthritis, lupus, and Sjögren’s syndrome)
- Inflamed eyelids and corneas
- Bacterial infection
Are you wondering if you might have MGD? There are myriad symptoms to help you identify the condition, though most of them overlap with dry eye.
In the early stages of MGD, you may not have any symptoms at all. Over time, however, they can begin to present themselves. Here are a few to be on the lookout for:
Are you wondering if you might have MGD? There are myriad symptoms to help you identify the condition, though most of them overlap with dry eye.
In the early stages of MGD, you may not have any symptoms at all. Over time, however, they can begin to present themselves. Here are a few to be on the lookout for:
- Red eyes
- A gritty sensation inside your eyes
- Itchy eyes
- Blurred vision
- Inflamed eyelids
In addition, your low oil levels may be due to medications you’re currently taking.
For instance, if you’re on estrogen replacement therapy medication or drugs meant to reduce androgen hormones, your eyes may be drier than usual. This is also the case if you’re using retinoids or any other anti-aging skincare that may drip into your eyes.
Trigger Factors
Do you spend a large part of your day on the computer?
Do you live in an arid environment with dry air pumping in your home or office?
If so, you could notice that your MGD symptoms worsen in his atmosphere.
In some semi-rare cases, you may also notice a rough and uneven surface along the inner rim of your eyelid. Not everyone has this unevenness, so it’s always important to call your eye doctor to determine what you’re looking at.
In the same vein, though it’s tempting to self-diagnose, always consult your eye doctor before beginning treatment for any eye-related condition. Failing to do so could exacerbate your symptoms rather than mitigate them.
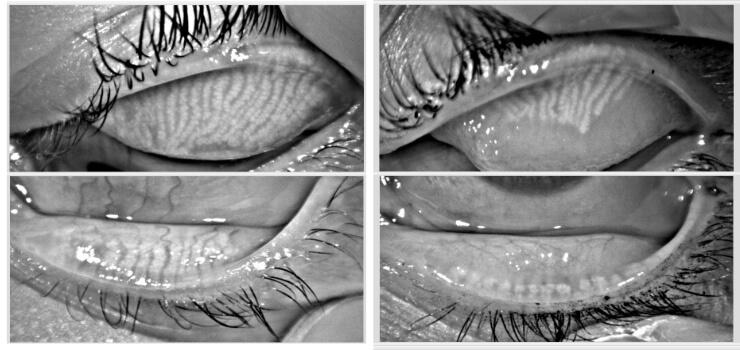
How can your eye doctor test for MGD?
Your eye doctor can look at the glands and their shape. Your doctor can also look at how well they make oils.
Your doctor will examine the level and content of the oil production to help determine if MGD could be the underlying cause of your dry eye symptoms.
Tear Breakup Time Test
Your doctor can also examine the contents of your tears as a diagnostic measure, analyzing their stability, quality, and quantity.
If this is the route taken, your doctor will perform what’s known as a tear breakup time test, or TBTT. They apply a small amount of dye to the front surface of your eye, on your tear film.
Then they perform an eye exam using a special cobalt blue light. Why blue? It makes your tears glow!
During this painless exam, your doctor can measure how long it takes for your tears to break down. In other words, what’s their stability level? This can help lead to an MGD diagnosis or dismissal.
Tear breakup time can also be measured without dyes. This is called Non-Invasive Tear Breakup Time. This test uses an infrared device (e.g. Oculus Keratograph 5M) to measure how rapidly your normal tears begin to evaporate.
Meibomian Gland Evaluation
A Meibomian Gland Evaluator (MGE) is a simple device shaped like a USB stick. It has a spring inside at a certain level of pressure. It replicate the force of a normal blink.
The MGE gently touches the lower eyelid edge. A tiny amount of pressure is applied to see how much oil comes out (and whether it is clear or thick and pasty). The thicker and cloudier the oil, the more Meibomian Gland Dysfunction is present.
Effective Treatments for MGD
Warm compresses and eyelid cleansers are common treatments for MGD.
When done everyday, warm compresses can allow warmth into your Meibomian Glands. This helps to keep oils from clogging.
Looking for more at-home remedies you can use while you wait for your eye doctor appointment? Here are a few more tips.
Eyelid cleansers
Did you know that your eyelids have bacteria on them? We’re born with bacteria on our skin. On the eyelids, these bacteria can overgrow. They eat the natural oils of your eyes and throw junk in them. Look for hypochlorous acid sprays or okra-based cleansers. The latter can also kill mites called Demodex.
Eyelid Massage
Ever heard your parents say to stop rubbing your eyes? Eyelid massage is the same. It is generally not recommended, unless via an eyecare professional.
Choosing Cleansers and Cosmetics
It’s best to be as gentle on your eyes as possible, especially if you’re suffering from MGD. Avoid irritating soap cleansers and instead, use a natural non-soap alternative to wash your face.
As you cleanse, avoid getting any solution on or around your eyes. Instead, use a makeup remover to get rid of all traces. You should also avoid touching your fingers or cotton pad near your eyes when you apply skincare products containing retinol on your face.
Looking for a good mascara? Check out this review of mascaras and the best mascara for sensitive eyes.
Adding Moisture To the Air
If you can attribute your dry eyes to your climate or your home’s HVAC unit, try running a humidifier at night. This adds moisture into the air and can counter any damaging effects of indoor heating and air conditioning.
Let’s take a look at five modern treatments that are changing the game.
Newer Treatments for Meibomian Gland Dysfunction
- Intense Pulsed Light
Intense Pulsed Light helps to switch on your Meibomian Glands. This helps them to be younger and more active. Over a series of treatments, your doctor can see your glands work better. This may mean that you go from thick, toothpaste oil to runny olive-oil-like oil.
- Prescription Anti-inflammatory Eye Drops
If you’ve ever grabbed a bottle of Xiidra or Restasis, you know it can be a helpful addition to your dry eye regimen. Anti-inflammatory drops helps enhance your eyes’ natural ability to create tears. It does this by altering your body’s immune system response so you’re more prone to tearing.
- Antibacterial Eye Drops
For some people who suffer from MGD, antibacterial eye drops are all they need to keep the symptoms at bay. While there is some merit to this approach, researchers require more advanced studies before they can draw a direct connection of healing.
- Omega-3 Supplements
Healthcare professionals around the world have long heralded omega-3 supplements for the nutritious fatty acids they contain. Your doctor might recommend that you start a diet focused on foods rich in omega-3s to help improve your tear function. You can find omega-3s in salmon, walnuts, eggs, bread, spinach and more! Keep in mind that these supplements aren’t meant to replace one of the above steps, but to complement it. Stick with the plan you received from your doctor, adding in the changes when possible.
- LipiScan and LipiFlow LipiFlow is an in-office treatment that gives comfortable warmth to your meibomian glands. This encourages them to loosen any thickened oil. In a recent scientific review, Lipiflow made significant improvements to dry eyes and the normal flow of oil from the glands.
Find Your Next MGD Doctor Today
When your eyes are dry, even the most simple task can seem like an overwhelming chore. Between the burning and itching, it can be difficult to make it through the day.
The good news? There’s no shortage of treatment options designed to help you treat your Meibomian Gland Dysfunction.
When you’re ready to find the best dry eye clinic near you, let us help.
Browse the specialties, locations and more to find one that’s a good fit. Then, feel free to make an appointment. Take that first step together!

